RESEARCH IN THE BRANDT LAB
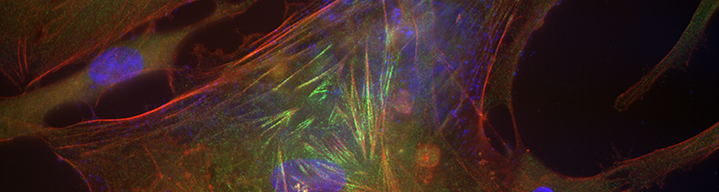
Herpes simplex virus (keratitis) is the leading cause of blindness due to infection in the US with about 24,000 new cases per year. Initially, the virus infects epithelial cells in the cornea, and usually resolves without affecting vision. At the same time, the virus enters sensory nerve endings in the cornea and travels through the axons to establish a latent infection. Periodically, the virus reactivates and travels through the axons back to the cornea inducing recurrent keratitis and immune-mediated damage can increase with each reactivation episode. HSV keratitis is an immunopathological disease. Ultimately, the cornea becomes cloudy with ingrowth of new blood vessels and the only therapy is a corneal transplant. Because trafficking through nerve axons is critical, our lab has begun to focus on how the transport is regulated. Trafficking occurs on microtubules and is known to require dynein and kinesin proteins but there are numerous microtubule associated proteins (MAPs) in cells that regulate the process. Little is known about how these MAPs regulated HSV trafficking and one goal is to identify MAPs that are involved and study their mechanisms of action.
Another component of HSV keratitis is the retraction of sensory nerves from the cornea and is referred to as neuronal keratopathy. Previous studies have suggested that the immune response is at least partially involved but the mechanisms are not known and events occurring in the nerves themselves have not been explored. One mechanism is the process known as Wallerian Degeneration, where axons develop blebbing and fasciculation and eventually wither. We have developed a cell culture model of WD and are investigating several parameters of infection that could lead to WD.
Gene delivery to the eye is restricted by the volume that can be injected. For efficient gene delivery, one must have very high titer stocks of vector virus (not obtainable with some vectors). Every cell has intrinsic host resistance factors that block virus infection, thus, transient interference with these factors could improve delivery efficiency. We have shown that knock down or chemical inhibition of these factors improves gene delivery in the eye or ocular cells and are investigating the mechanisms involved. Viral-mediated gene delivery to non-human primate eyes results in transient uveitis. Even though this clears in 7 to 10 days, it is an unwanted side effect. We are working to identify the induction mechanisms with the goal of ultimately blocking the inflammation. This has led to the characterization of innate immune signaling systems in primate ocular tissues. We do not see the same effect in rodent eyes indicating there are fundamental differences in these systems between rodents and primates.
Finally, we subcontract with drug companies to test potential antimicrobial drugs both in cell culture and in animal models and have worked with numerous companies over the years testing a wide variety of small molecules, peptides, and antibodies.